Feeling Dismissed and Ignored by Your Doctor? Do this.
By Helene M. Epstein

Diagnosis is a journey. Over the next few months, this column will take you through the various steps of that journey to help you get an accurate diagnosis. Last month we focused on the most important questions to ask when you get a working diagnosis. Each month we’ll show you where the pitfalls may be, how to be proactive, and how to partner with the healthcare team to reduce your risk. [If you want an overall look at how misdiagnosis happens, click here.]
Trust is an essential part of healthcare. When we feel poorly, we visit our doctor with our hopes high, trusting that she will help us heal. We bring her our concerns, our list of symptoms, our history, and our questions. In exchange, we expect answers, or at the very least an effort to find answers.
What if we feel like our trust isn’t returned? What if our symptoms are dismissed or our story considered unlikely? What do we do if we feel strongly in our gut that something is wrong despite the medical expert who says we’re fine and we can go home? Or we’re told it’s just stress, or a touch of the flu, or a common childhood illness? Or the worst dismissal heard by so many: it’s all in your head?
Being ignored by your healthcare professional is one of the most common complaints heard by patient advocates, healthcare reporters, and now social media. Twitter blew up last month with the hashtag #PatientsAreNotFaking in reaction to a video by a nurse making fun of a “patient” (played by the nurse) exaggerating her symptoms. Over 77 thousand patients tweeted delayed diagnosis stories in just the first week. While we don’t know the details of these stories, the passionate tweets displayed the amount of fear, anger, and harm that a breach of trust can cause. When we visit our healthcare professional at our most vulnerable, learning that our symptoms are being discounted hurts. The impact can cause both emotional and practical damage. Too often dismissed patients avoid health checks in the future and go without proper medical care and screenings.
There is a subtle difference between a patient who experiences a delayed diagnosis and one whose symptoms are dismissed. Delay can happen for many reasons. The difference may be as simple as having a doctor or nurse who asks you to return if your symptoms change or become worse.
Dismissed patients share a more nuanced tale. They are not believed, or they’re told they’re overreacting. They’re accused of exaggerating their symptoms or pain. Or they suggest something that the doctor considers to be so far-fetched that the doctor-patient relationship itself is damaged.
Young doesn’t always equal healthy
Age bias comes in all shapes and sizes. Sometimes, a patient’s symptoms are dismissed because they are considered too young and generally healthy for the healthcare professional to even consider a serious illness. [Read the section “When parents’ concerns are dismissed”] Although these young patients’ symptoms weren’t dismissed, they all experienced diagnostic error because doctors didn’t expect that people their age could have these conditions or complications: Jessica Barnett, Alex Reed, John Michael Knight, and Rory Staunton.
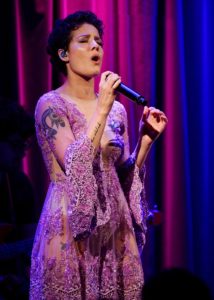
Halsey at the Grammy Museum.
Photo by Justin Higuchi/ CC BY 2.0
Young women with endometriosis frequently report being dismissed by doctors, even their gynecologists. Endometriosis is a common condition for women in their child-bearing years. It happens when endometrial tissue, usually confined to the lining of the uterus, is found in areas of the abdominal cavity outside of the uterus. The most common symptom is pain, and over time the condition can lead to scarring and adhesions. Teens and young women may suffer for a decade or longer before diagnosis and treatment. According to a major 2008 clinical study, “A surprisingly large number of the respondents… reported that their physicians had not taken them seriously overall or that they had been told that nothing was wrong sometime before diagnosis.”
Platinum-selling singer Halsey shared her endometriosis diagnosis with fans, letting them know she spent years in pain “with doctors essentially telling me I was being a big baby about my period” before getting diagnosed at 22. When a patient’s pain is discounted or ignored, it can have profound impact on their mental health. Halsey wrote, “Finding out I had endo was the most bittersweet moment because it meant I wasn’t crazy!”
When racial bias translates into medical bias
We know that many groups have higher rates of diagnostic error because of cognitive bias on the part of the healthcare practitioner: women, children, the obese, and the elderly all experience this. It’s unfortunately true across the board for people of color. They routinely do not get the same quality of care that white patients do, regardless of their level of education or financial resources.
Studies have shown that African-American patients have a greater tendency toward certain medical conditions, like inflammatory breast cancer, prostate cancer, lung cancer, and many others. Yet, they get screened at lower rates than white patients do. One issue that has received much needed media attention is the distressingly high rate of maternal mortality (death of a mother due to childbirth-related complications) for all U.S. women. Yet rates for Black women are three to four times higher than for non-Hispanic white women, often because their reported symptoms are not taken seriously. Studies on healthcare providers’ evaluations of patients’ pain levels also indicate that people of color are judged and treated with lower levels of concern and pain medicines than white patients are.
Stroke is another condition that hits African American women twice as often as white women, at younger ages, and more severely. Kimberly Rodgers didn’t have time to get ill: she was the primary caregiver for her father who had suffered a major stroke, was working a high-stress job, and attending graduate school in Chicago. When she began to experience migraines and sleep eluded her, she consulted her primary care physician. As an African American woman, especially one with a family history of stroke, her symptoms should have been taken seriously. Instead, she was told to see a nutritionist, get clinical massages and seek anger management counseling to relieve her stress.
A few months later, she developed new, alarming symptoms. She suddenly couldn’t see anything while driving her car on a highway. Though she recovered her eyesight, days later she developed a sudden sharp forehead pain and was unable to figure out how to work the washing machine. Her face looked strange to her in the mirror. She knew something was terribly wrong. Her aunt, a nurse, told her to get to the emergency room immediately.
Kimberly was having a stroke due to a blockage in her carotid artery. She recognizes now that there were several missed opportunities to catch it earlier. Her physician did not do a full physical exam, check her cholesterol, or discuss blood pressure treatments. Nor did the medical practice discuss risks and warning signs when Kimberly told them about her father’s stroke. When she came in with complaints about migraines and insomnia, they failed to consider stroke and missed the chance to order a simple, non-invasive ultrasound test that checks for blockages in the carotid artery. Kimberly recognizes she didn’t know enough to raise the issue herself.
She’s working hard to change that for the Chicago African-American community where stroke fatalities greatly outweigh other communities’. Kimberly sits on two boards for Northwestern Hospital, one focused on educating all minority communities and women about stroke, and the other seeking solutions for healthcare gaps for several conditions among minorities. She changed her graduate studies focus so she can educate adults of all genders and races about strokes and heart attacks. And she speaks about her journey, inspiring other patients to get involved in the diagnostic process.
Taking One’s Lumps
The expression “taking one’s lumps” means to stoically put up with an unhappy ongoing situation. In medical terms though, finding a lump means the possibility of “infections, inflammation, tumors or trauma.” So why were these patients’ lumps dismissed?
Jennifer Campisano, a SIDM Board of Directors member, found a lump in her breast when she was nursing her child. One doctor suggested it was an infection and prescribed Tylenol. The next one said it was nothing to worry about and suggested she could have it removed when she finished breastfeeding. Three months later, Jennifer sought the advice of a surgeon and a radiologist who biopsied her and diagnosed her with stage 4 breast cancer. She underwent years of chemotherapy. While someone was finally taking her symptoms seriously, they were still not completely correct. It turned out she had both an earlier stage breast cancer and sarcoidosis, an auto-immune disease that can mimic cancer. Jennifer’s dismissed lump was a complex combination of conditions, one that didn’t require the years of chemotherapy and its side effects. Reviewing her medical record, she learned that sarcoidosis had been suspected much earlier. However, because her tumor was so large the medical team feared the cancer could spread rapidly (metastasis) and started chemo immediately. Once chemo began, they were unable to test for sarcoidosis. Had she been tested before starting chemo her treatment plan would have been different; probably a mix of medications for the sarcoidosis and surgery/radiation for the breast cancer.
Pediatric neurologist Diana Cejas MD was a first year medical student when she discovered a small marble-sized lump in her neck. She was a second-year resident, five years later, when she was finally diagnosed. Despite the lump and Diana’s level of concern growing in size over the years, she was uncomfortable “making a fuss” about it. Part of her wanted all of the various physicians to be right; that the lump was nothing to worry about. Part of her concern was challenging the “power dynamic”, being a medical student, and later a new doctor, confronting more experienced attending doctors and experts.
Yet she couldn’t let it go, either. Every time she was examined, for any reason from annual check-up to a different medical concern, Diana would ask about the growing lump on her neck. She even saw a renowned specialist, who also told her to stop worrying. However, towards the end of her first year as an intern, her symptoms had changed and were impossible to ignore: dizziness, which she hoped was due to the long hours and pressures of being a first year resident, and waxing and waning needle-like pain, which soon became constant. She also noticed that the lump was large enough to be seen casually in photographs.
Finally, after a 28-hour shift and in pain that prevented sleep, she was determined to do something about it. Luckily, Diana was scheduled for a physical the next day. She described her symptoms to the primary care doctor as though she was presenting a patient on rounds to her attending: factual, detailed, and without emotion. She was surprised to learn that her constant questions about the lump had never been noted in her charts. Then she was dismayed when the doctor dismissed her symptoms again.
This time, she didn’t just accept the dismissal. “I was less angry than upset and I was just determined.” Diana says she told the doctor, “I’m not leaving here until we do something about this. So, to shut me up, she said, ‘We can get a CT (computed tomography) scan.’” She got the test, walked up two flights to return to the pediatric floor, and by the time she arrived on her floor, “my primary doctor was paging me.” It was a rare form of vascular tumor, a carotid body paraganglioma. Even rarer, it was malignant. Due to the long delay, and complications from the surgeries including stroke, Diana’s “lump” is gone but her own health was impaired.
Now, as a pediatric neurologist in North Carolina, Dr. Cejas listens closely to her patients and helps them find solutions. She also advocates for people with disabilities, by speaking on the topic and sharing her own story.
What you can do if your symptoms are dismissed or ignored
All of these stories offer us valuable lessons. If you feel that your healthcare professional isn’t really listening or heeding your concerns, there are many steps you can take to get the answers you seek. Here are a few suggestions:
- If your symptoms are ignored, ask, “What might this be?” And then ask, “What do I do if these symptoms get worse?” These type of questions help the doctor to stop and consider the options. Learning from Jennifer’s story, you might want to phrase it as, “What else might this be?” Just because you have one established condition, doesn’t mean that you can’t have a second issue that needs independent investigating.
- Try to find a medical practice you can trust. Healthcare professionals are under severe time constraints but that doesn’t mean they shouldn’t have time to hear their patients’ reasonable concerns and goals. If you feel that your doctor or nurse-practitioner is consistently ignoring what you have to say, even if your symptoms continue to progress, find another primary care practice.
- If you feel your primary care doctor doesn’t take your symptoms seriously, ask for a referral to a specialist or go to a different practice for a second opinion. A fresh set of eyes can be extremely helpful.
- Review how to present your symptoms factually, clearly, quickly, and without unnecessary minutiae. Sometimes symptoms aren’t ignored by the doctor, they’re just lost in a list that’s too long or includes what the clinician feels are irrelevant details. Ask them how to best present the information. Most importantly, put your symptoms into context.
- Learn about the types of screenings that should be performed routinely for patients of your age, gender, and race. Here is a link to a document that lists preventative screenings for adults by these criteria. Discuss it with your medical practice. If they refuse to do the relevant routine screenings, seek another medical practice that is more conscientious and aware of why different genders, ages, and races have different medical concerns.
- Speak up. Diana Cejas recognizes that her reluctance to share the depth of her concerns played a part in how long it took her to get diagnosed. However, she knows that many patients feel uncomfortable asserting themselves to doctors. Dr. Cejas says, “Be willing to fight for yourself and your body but don’t be willing to put on the boxing gloves” when you first walk in. Instead, she recommends you ask for help figuring out how to deal with your symptoms now and eventually find the cause of those symptoms.
- While it is important to learn about your symptoms from reliable sources, doing so doesn’t mean demanding specific tests or treatments for some rare disorder you haven’t been diagnosed with. Dr. Cejas recommends asking for help in dealing with your symptoms politely yet firmly.
The Society to Improve Diagnosis in Medicine (SIDM) catalyzes and leads change to improve diagnosis and eliminate harm from diagnostic error. We work in partnership with patients, their families, the healthcare community, and every interested stakeholder. SIDM is the only organization focused solely on the problem of diagnostic error and improving the accuracy and timeliness of diagnosis. In 2015, SIDM established the Coalition to Improve Diagnosis, to increase awareness and actions that improve diagnosis. Members of the Coalition represent hundreds of thousands of healthcare providers and patients—and the leading health organizations and government agencies involved in patient care. Together, we work to find solutions that enhance diagnostic safety and quality, reduce harm, and ultimately, ensure better health outcomes for patients. Visit our website at www.improvediagnosis.org, and follow us on Twitter or Facebook.
Helene M. Epstein writes about patient safety and family health. Her goal is to help readers apply important new information to their own lives. Subscribe to her website at www.hmepstein.com and follow her on Twitter, Facebook, and YouTube.
Dx IQ is made possible with funding from the Mont Fund and the Gordon and Betty Moore Foundation.

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Republish our Dx IQ articles for free, online or in print, under Creative Commons license. Please do not edit the piece. Ensure that you attribute the author and mention that the article was originally published by the Society to Improve Diagnosis in Medicine. If you republish, we’d love for you to let us know by sending an email to info@improvediagnosis.org.
Resources for Patients
At SIDM, we are focused on raising awareness about the magnitude and impact of diagnostic errors as providing tools and resources to equip patients to participate in achieving an accurate and timely diagnosis.




