Medical testing’s dirty little secret and how you can protect yourself
By Helene M. Epstein

Diagnosis is a journey. Over the next few months, this column will take you through the various steps of that journey to help you get an accurate diagnosis. Last month we focused on what to do if your symptoms are dismissed or ignored. Each month we’ll show you where the pitfalls may be, how to be proactive, and how to partner with the healthcare team to reduce your risk. [If you want an overall look at how misdiagnosis happens, click here.]
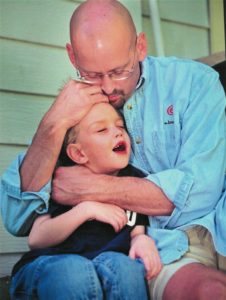
Patrick Sheridan was relieved to hear he didn’t have cancer. The initial report on the tumor removed from his spine said it was benign. However, no one at the neurosurgeon’s office was aware that corrected test reports were neither seen by the surgeon nor communicated to Pat. Six months later, when his pain returned, Pat and his doctor learned that the unseen test results noted he had an aggressive, malignant sarcoma requiring urgent treatment. It was too late and Pat died when he was 45.
Sarah Boyle was just 25 when she had months of chemotherapy followed by a double mastectomy for her invasive breast cancer. That’s when she learned she never actually had breast cancer. The lab’s official statement blamed “human error” for misdiagnosing a cancer-free patient with invasive cancer. Despite enduring difficult and unnecessary treatment and surgery, today Sarah is focused on helping prevent this kind of error for others.
Medical testing should only happen after a complete history is taken and a physical exam is given. It can be an essential step in getting properly diagnosed. Though the vast majority of tests are conducted correctly, and reported quickly and accurately to the healthcare professional and the patient, understanding how the testing process can and does go wrong can give you an opportunity to protect yourself.
Think of medical testing as a relay race of sorts with your test sample passing from one person to another. With every handoff, in every step, there is the possibility of an error in the care and handling of your sample or the analysis of your test. As a patient, you have an important role to play starting with preparing for every test. As we covered in an earlier column, ask “What do I need to do to prepare for this test?” Many tests are impacted when you don’t follow the instructions to the letter. With so many opportunities for error, what should you watch for and what can you do about it?
Closing the Loop on Test Results
You can’t be treated for a health condition no one knows you have. It is surprisingly common for healthcare professionals –– and the systems and organizations that are supposed to serve them –– to fail at following up on essential test results. Closing the loop means to complete the testing process correctly, so that everyone who needs to know what the tests show has the information to act on. Each person who handles your test samples and results has a process to follow to make certain that the information gets to the doctor and ultimately to the patient. However, as Patrick Sheridan’s story demonstrates, there is no guarantee. Sometimes, the patient and the healthcare professional don’t know there’s a test report they haven’t seen.
What you can do:
- Join the patient portal. Most primary care practices now have patient portals, which are online websites with high security. You can log in to see and print your test results, email general questions to the doctor, double-check that your health history information is correct, and update incorrect or old information. Yours may even allow you to make appointments or share information with other medical practices. Many specialty practices still aren’t offering them. Ask if they have one and how you can join.
- Keep notes. In November 2019’s column, we suggested seven essential questions when tests are ordered. Write down the answers for every test you are given, when it was done, how the results will be communicated, and when the results are due. There can be different timelines for different types of tests, so you need to ask about each one. Results from an imaging test can be in the doctor’s hands as soon as the next day while cultures can take a week or more. We recommend marking this info in your calendar. For example:24-hour urine test, conducted at home, dropped off at lab 12/5/2019, office will call if results are abnormal, results expected 12/12/2019, call on 12/13/2019 if you don’t get results before.
- Follow-up. You can help close the loop. If you don’t hear from the doctor or see the results posted in your patient portal within a day or two after the due date, call them. Remember no news is no news. Patrick Sheridan got the initial biopsy results but didn’t know that there would be a more detailed follow-up. Despite his neurosurgeon’s office mishandling of the information, a call could have revealed the important information in the missing report.
What others are doing: Doctors and nurses are also dissatisfied with their systems’ level of failure managing outpatient test results, perhaps as much as patients are. So, healthcare groups are looking for solutions to help close the loop on test results. There are quality improvement initiatives happening all across the United States.
Test results that haven’t been seen by the doctor or the patient is a persistent patient safety problem. So, in December 2018, the state of Pennsylvania passed a new law that may help. Imaging centers (MRIs, CTs, etc.) must notify patients directly within 20 days when a test result requires follow-up by a physician. This law is what’s known as a work-around, a patch method for preventing mistakes that shouldn’t happen in the first place. Being aware of what specific tests you are taking and when you should hear the results is a work-around too but one that puts you in control of your own information.
Understanding Test Results
When tests are ordered, it is usually because the healthcare professional thinks these tests may shine a light on your diagnosis, the cause of your symptoms. She has thousands to choose from. Blood and urine tests are often grouped in panels so one sample may return many results.
 Few tests have simple “Yes” or “No” answers. Most lab tests are compared to an established reference range from healthy people. When your test outcomes are reported, you’ll learn if your results are higher, lower, or similar to that range. For example, your cholesterol count may be deemed low, normal, or high. A high cholesterol result can suggest a risk for heart disease in the future. Therefore, it may lead to a treatment plan of diet and exercise, or the doctor may also prescribe medication for helping to lower your cholesterol. If your cholesterol is low or normal (within the reference range), she might not even mention it.
Few tests have simple “Yes” or “No” answers. Most lab tests are compared to an established reference range from healthy people. When your test outcomes are reported, you’ll learn if your results are higher, lower, or similar to that range. For example, your cholesterol count may be deemed low, normal, or high. A high cholesterol result can suggest a risk for heart disease in the future. Therefore, it may lead to a treatment plan of diet and exercise, or the doctor may also prescribe medication for helping to lower your cholesterol. If your cholesterol is low or normal (within the reference range), she might not even mention it.
Test results can be misleading to both your doctor and you. The reference ranges represent typical patients, but not everyone. Also, some autoimmune diseases, like rheumatoid arthritis (RA) or Lyme Disease, are plagued by negative results. Patients who suffer from that condition but test negative can wait years for a diagnosis. For example, there are blood tests that can help diagnose RA, looking for measurable levels of an inflammatory marker called rheumatoid factor. Only 85 percent of RA patients ever test positive for that factor, and many patients don’t. Furthermore, some people without RA can have a positive rheumatoid factor. To make an accurate diagnosis, the doctor needs to rely on a whole host of information. Family history, which joints are involved, when it began, how long it lasts, are all clues to an RA diagnosis.
To learn more about reference ranges and what your test results mean, visit the American Association for Clinical Chemistry (AACC)’s website.
What you can do:
- Get the report: Having a copy of your results helps you feel secure that the report has finished its relay race into your hands plus it gives you a chance to learn more. There are lots of ways to do this. When you take a lab test or imaging test, request a full copy of the report. The staff at your medical practice and the testing facility can tell you how to get it. There is a federal directive that commercial labs are required to give you a copy of your test results if you ask for them although you may have to wait or even pay for it. Several lab testing organizations (such as Quest and LabCorp) have their own patient portals that make it easy to get results. Some medical practices will contact you to discuss the results before sending them to you or posting them on the patient portal where you can download and print a copy.
- Read the report. The reports are written for healthcare professionals, not patients, but there is a lot you can learn by reviewing them. Some of the information will be easy to understand although much of it will be clear as mud. Don’t stress about it. Help is easily available.Imaging reports are written by a radiologist and include her conclusions. To make sense of it, you can visit a very helpful website run by the Radiological Society of North America, Inc. (RSNA). They explain the different types of tests and help you to read and understand your imaging test report. They also have a thorough A-to-Z list of tests and medical conditions.Lab reports usually have clearly marked columns organized by the type of test, the result, the reference range (often labeled as “Limit”), and the unit of measurement. There is also a very important column, often titled “Flag.” That’s where you see which test results are outside the typical range for healthy patients. Visit AAAC’s website LabTestsOnline.org to learn how to read your lab report. It has lots of information about the lab tests you’ve been given, and about different types of tests by medical condition.
- Discuss the results with your healthcare professional. It’s okay if you have questions after reading the reports even if your doctor has already called you to discuss the results. Sometimes the report cites out-of-range test results the doctor didn’t mention. Contact the office to request a phone call or a follow-up appointment. You can also use the portal to send a message to the doctor with your questions. Each medical practice has a preferred way of communicating. Ask them what’s the best way to get the answers you need.
Inaccurate Test Results
Here’s a scary thought. What if the test result is wrong? That’s what happened to Sarah Boyle. A false positive means that you might get treated for a condition you don’t have. A false negative means that your medical condition will go untreated until your symptoms worsen.
Why are some test results wrong? The reasons are tied to the type of test, who or what is analyzing it, reference range issues, and often how the test is done. Here are a few ways that incorrect test results can happen.
There are three phases of lab testing: pre-analytical, analytical, and post-analytical.
 Pre-analytical. The vast majority of known lab errors — 46 to 68 percent — happen in the pre-analytical phase. Mishandling samples, ordering the wrong test, mixing up patients’ names on the sample, or incorrect preparation by the patient are a few examples. Even your blood pressure reading can be inaccurate. Were you running late? Ask for a moment to breathe deeply and relax. Use the bathroom before and don’t drink a lot of water. A full bladder and being overhydrated can artificially raise blood pressure. If you get stressed when the nurse weighs you, ask to do it after the blood pressure reading. Sit straight, feet on the floor, and don’t speak until after. The technician can also make mistakes. Look at this article for a peek at what errors emergency medical personnel may make.
Pre-analytical. The vast majority of known lab errors — 46 to 68 percent — happen in the pre-analytical phase. Mishandling samples, ordering the wrong test, mixing up patients’ names on the sample, or incorrect preparation by the patient are a few examples. Even your blood pressure reading can be inaccurate. Were you running late? Ask for a moment to breathe deeply and relax. Use the bathroom before and don’t drink a lot of water. A full bladder and being overhydrated can artificially raise blood pressure. If you get stressed when the nurse weighs you, ask to do it after the blood pressure reading. Sit straight, feet on the floor, and don’t speak until after. The technician can also make mistakes. Look at this article for a peek at what errors emergency medical personnel may make.
Analytical. What may be the biggest problem in clinical lab testing has been difficult to measure: the analytical phase for “waived” lab tests. These common, high-volume tests are considered foolproof but that’s only true if the testers follow the manufacturer’s instructions to the letter. The government stopped inspecting or supervising labs licensed to provide these tests in 2002. The tests and the labs conducting these tests are literally waived from oversight. Over 200 supposedly simple tests can be conducted by people with little or no training. Over 150 thousand labs offer these tests. It’s important to note that we’re not referring to hospital or reference labs which handle complex tests, are closely supervised, and are known to be highly accurate.
In 2014 a spot check uncovered issues in over half of the labs reviewed. They found major issues like using expired products, mishandling chemicals, not following manufacturer’s directions, and unclean conditions. Of course, that doesn’t mean that half of the tests were mishandled. It means that waived testing labs are run by people and mistakes have been made. The concern is we don’t know what the impact of these mistakes has been because no one is measuring it. The list includes important and common diagnostic tests like pregnancy, diabetes, cholesterol, urinary tract and strep infections, and HIV tests.
Human error also plays a part in pathology and imaging tests. This may be what happened to Sarah Boyle. One study reviewed many forms of imaging tests. It concluded that radiologists’ accuracy drops after long shifts or reviewing too many images. According to a study of over 100 pathologists in eight states, one-in-four breast tissue biopsies tested for cancer may be read incorrectly.
Other studies have demonstrated, in the words of one astonishing report, “that where a patient obtains [an] MRI examination and which radiologist interprets the examination” can directly impact the diagnosis, treatment, and outcomes. In this study, one woman’s spine was scanned at ten different accredited MRI centers in the New York metro area over a period of three weeks. The centers didn’t know this was a test so she was treated as a typical patient. The results varied widely from one another. The average false negative rate — meaning they missed reporting on something that was known to exist — was 43.6 percent. The authors called it “an alarmingly high number of interpretive errors in the lumbar MRI reports.”
Post-analytic. The post-analytic phase includes communication of the results among the testing center, the medical practice, and the patient; as well as the doctor’s review and interpretation of the results.
Errors can occur if your race, gender or age is different than what was used for the specific test’s reference range. According to a 2015 study, researchers have known since the early 1970s that there are racial/ethnic differences for some laboratory tests. Yet, no racial/ethnic-specific reference ranges have been created. That applies to gender differences as well. Transgender patients take hormone treatments that can affect many tests. They need their own reference range, too.
What you can do: It all sounds overwhelming but there are steps you can take to help reduce potential errors in the testing process.
- Double-check what you can. Is your name and birthdate on the urine sample before you close the lid? Ask to see the labels on the vials of blood to check those, too. If your tests are done at another facility, make certain that what they’re testing is what you’re expecting. Read the forms and feel comfortable asking questions before you sign. When you read your lab reports, do you see the phrase “Test Cancelled” or “No Specimen Received”? Ask your medical practice what happened. Follow all of the instructions you receive before the test so you don’t accidentally make the results invalid. Stop eating if and when they tell you to or stop taking the supplements or medicines they tell you to avoid. If you realize you made a mistake, fess up and ask for a test to be redone. Double checking also applies to ensuring every test you took is matched with a result and that you have received and read it.
- Advocate for yourself. You have access to lots of reliable, informative websites with helpful information about your symptoms. If your healthcare professional dismisses your symptoms because the test results are all normal, remind him that your symptoms still exist. You can also ask if he was surprised by any of the test results and if he would consider other relevant tests or retesting. At the very least, ask what the next steps are.
- Pay attention to your symptoms: Even if your test results don’t explain your symptoms, keep track of them just as you did before seeing the healthcare professional. It may be nothing important or it may be an essential clue to a delayed diagnosis and treatment. Now that you know testing error can occur, recognize that your condition may have been missed or that your condition may still be in its early stages and not measurable, yet.
- Always get a second opinion before any planned surgery due to test results. Get tests redone at a different lab if you’re told you have a serious or life-threatening condition. Have tests rerun elsewhere before beginning any high-risk treatment plan. It’s worth the extra few days and dollars.
- Ask the imaging center where you will get a mammogram, MRI, CT scan, or ultrasound if the test is automatically reviewed by two radiologists before it’s reported. If not, ask if a review can be requested after getting your results. Most will do so if the ordering physician does so; some if the patient requests a second opinion.
What others are doing. Researchers are always looking for more reliable diagnostic tests. It takes time for these new tests to be proven accurate and used by healthcare professionals, usually years. Also, every year, we learn that certain tests are flawed and results need to be carefully reviewed. Getting that information to every doctor and nurse takes time.
Remember, for most patients, the testing process is successful. Now that you are aware of how it could break down, feel reassured that you have a role in getting an accurate diagnosis. Speak up, ask questions, ask more questions if you need to, and participate in ensuring that nothing gets missed. Please share this so your friends and family can do the same.
The Society to Improve Diagnosis in Medicine (SIDM) catalyzes and leads change to improve diagnosis and eliminate harm from diagnostic error. We work in partnership with patients, their families, the healthcare community, and every interested stakeholder. SIDM is the only organization focused solely on the problem of diagnostic error and improving the accuracy and timeliness of diagnosis. In 2015, SIDM established the Coalition to Improve Diagnosis, to increase awareness and actions that improve diagnosis. Members of the Coalition represent hundreds of thousands of healthcare providers and patients—and the leading health organizations and government agencies involved in patient care. Together, we work to find solutions that enhance diagnostic safety and quality, reduce harm, and ultimately, ensure better health outcomes for patients. Visit our website at www.improvediagnosis.org, and follow us on Twitter or Facebook.
Helene M. Epstein writes about patient safety and family health. Her goal is to help readers apply important new information to their own lives. Subscribe to her website at www.hmepstein.com and follow her on Twitter, Facebook, and YouTube.
Dx IQ is made possible with funding from the Mont Fund and the Gordon and Betty Moore Foundation.

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Republish our Dx IQ articles for free, online or in print, under Creative Commons license. Please do not edit the piece. Ensure that you attribute the author and mention that the article was originally published by the Society to Improve Diagnosis in Medicine. If you republish, we’d love for you to let us know by sending an email to info@improvediagnosis.org.
Resources for Patients
At SIDM, we are focused on raising awareness about the magnitude and impact of diagnostic errors as providing tools and resources to equip patients to participate in achieving an accurate and timely diagnosis.