Policy Roadmap for Research to Improve Diagnosis
Public Health Imperative
The Human Toll and Financial Costs of Diagnostic Error
The Problem
A critical area of patient safety, healthcare quality, and cost savings that has not been adequately addressed by the healthcare sector is the issue of reducing diagnostic errors.
- Diagnostic errors affect more than 12 million Americans each year and may seriously harm one third of these patients, likely dwarfing all other causes of harm from medical errors combined.
- At a minimum, diagnostic errors cause more serious harms to patients than any other type of medical error, and 40,000 to 80,000 die each year from diagnostic failures in U.S. hospitals alone.
- Costs are driven up by treating sicker patients (after the fact) in more advanced disease states, protracted “diagnostic journeys,” and by the overuse of unnecessary, expensive diagnostic tests.
- Improving the accuracy and timeliness of diagnosis will reduce costs from inappropriate testing, wrong treatments, and malpractice lawsuits, potentially saving over $100 billion per year.
- According to the National Academy of Medicine, "Improving the diagnostic process is not only possible, but also represents a moral, professional, and public health imperative."
According to the National Academy of Medicine (NAM), diagnostic errors represent a major public health problem likely to affect each of us in our lifetime. The 2015 NAM report on Improving Diagnosis in Health Care calls us all to action with the powerful statement, “Improving the diagnostic process is not only possible, but it also represents a moral, professional, and public health imperative.”
Annually in the U.S., there may be more than 12 million diagnostic errors with one in three such errors causing serious patient harm. The aggregate annual costs to the U.S. healthcare system could be as high as $100 billion/year. Despite its enormous toll on human lives and massive drain on societal resources, opportunities to improve the diagnostic process have been largely ignored in prior patient safety and quality efforts. This is mostly because the problem remains largely hidden—diagnostic errors are rarely evident when they occur, and only surface at a later time when misdiagnosis-related harms have already occurred. Diagnostic errors represent the bottom of the iceberg of patient safety.
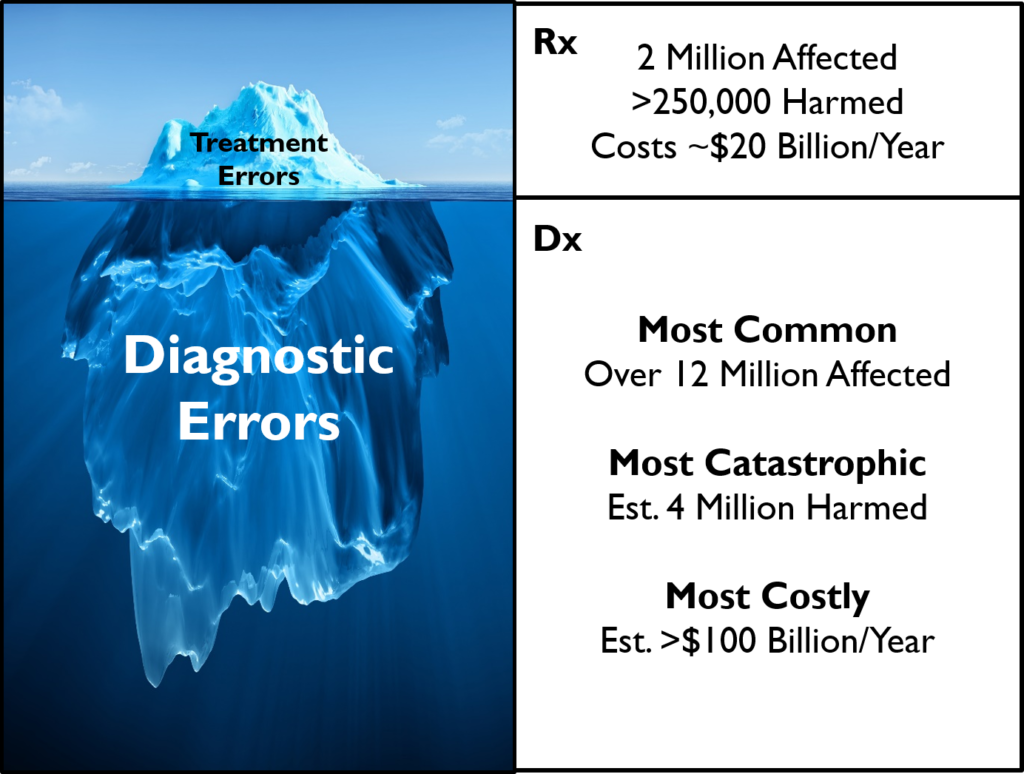
Diagnostic errors are the bottom of the iceberg of patient safety. Treatment (Rx) errors have a major public health impact, but diagnostic (Dx) errors have an even bigger one. Physician errors resulting in adverse events are more likely to be diagnostic than drug-related (14% vs. 9%); tort claims are nearly twice as common as claims for medication errors and result in the largest payouts; diagnostic errors are more likely to result in serious disability (47% vs. 14%).However, because diagnostic errors are discovered in hindsight and not routinely tracked, they remain hidden.
Causes and Solutions
The Need for More Research
The science of improving diagnostic safety and quality is still nascent. The lack of research funding is directly responsible for limited progress. This under-resourced area presents a dramatic opportunity for early return on investment.
- Diagnostic errors must be solved in a scalable way through a systems improvement framework. Making progress will require significant investment to understand burden, causes, and solutions.
- Progress on these issues has been hampered by the lack of Federal research funding for this topic and a lack of research capacity (e.g., access to key data and adequately trained researchers).
- Relative to its public health footprint, diagnostic errors are likely the most underfunded research area in medicine, directly receiving only about $7 million per year. Many individual diseases with smaller public health impact receive orders of magnitude more funding each year.
- The National Institutes of Health (NIH) has a disease-oriented funding structure that serves research on disease mechanisms and treatments well, but research on diagnosis poorly.
- The Agency for Healthcare Research and Quality (AHRQ) has a strong mission-aligned interest in this area, but limited funding to accomplish ambitious and important quality and safety goals.
There is no single cause and no single solution to the problem of diagnostic errors. The NAM defines diagnostic error broadly as “the failure to (a) establish an accurate and timely explanation of the patient’s health problem(s) or (b) communicate that explanation to the patient.” Missed, wrong, and delayed diagnoses often result from cognitive errors linked to knowledge gaps, provider inexperience with specific problems, or biased human reasoning. Others result from failures in care coordination, communication, or reporting of test results. These problems must be solved in a scalable way through a systems improvement framework, but achieving this requires a robust pipeline of diagnostic research.
Ultimately, diagnostic errors represent failures of our healthcare delivery system in the broadest sense. While many of these “errors” are linked to individual physician actions, this does not imply negligence on the part of any specific provider, and fixing the diagnostic process requires a holistic view of the system. The “system” here refers to all of our healthcare delivery structures and processes, including the diagnostic education, training, and certification of providers; electronic tools supporting the delivery of day-to-day care; payment models that affect how we value and incentivize correct, timely diagnoses; and government research infrastructure and total funding dedicated to improving diagnosis. The diagnostic process must be addressed using multifaceted, transdisciplinary, team-oriented solutions developed within a systems science framework. As the NAM report articulated, because diagnostic quality and safety research remains underfunded and the science underdeveloped, improving diagnosis for patients requires critical further research to develop, refine, and fully implement such solutions.
There is now ample evidence that we are not yet doing enough research on this critical topic. A recent systematic review of the medical literature found many potential solutions, but almost none that have yet been studied in actual clinical practice to determine whether they improve patient outcomes. The 2015 NAM report clearly identified the need for further research and called for “dedicated funding for research on the diagnostic process and diagnostic errors” as one of its eight final recommendations. A 2017 study estimated that US Federal research spending targeted towards tackling the diagnostic error problem remains minimal, totaling just a few million dollars each year. It is notable that the total spent on diagnostic error-related research is substantially less than what we now spend each year for federally-sponsored research on individual diseases, most with much smaller public health impact.
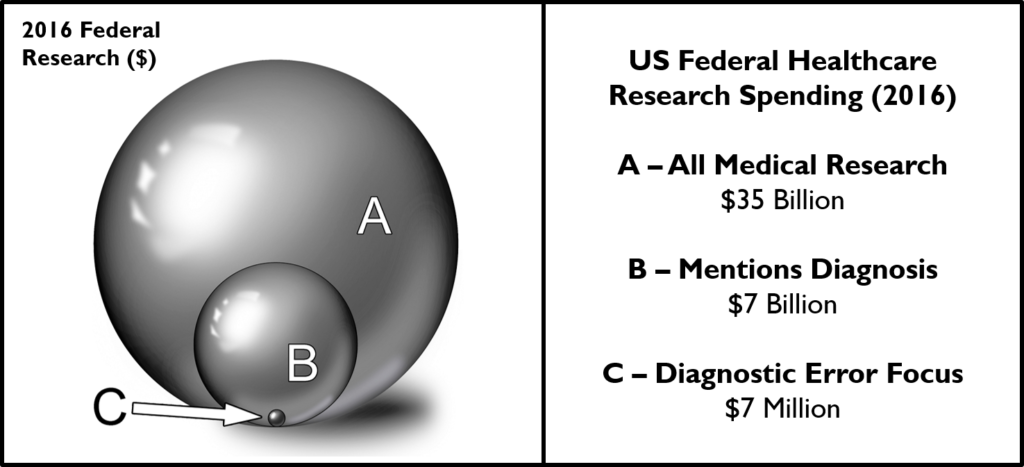
Diagnostic errors research funding is woefully inadequate. Treatment-related research (basic, translational, and clinical) receives the vast majority of federal healthcare research dollars. Even after the 2015 NAM Report Improving Diagnosis in Health Care, federal agencies involved in medical research spent just 0.02% (~$7 million) of their aggregate budget (~$35 billion) on issues related to improving diagnostic quality or safety.
