To motivate and help hospitals improve diagnosis, Leapfrog to pilot-test 29 recommended practices
By Susan Carr, Senior Writer
Although awareness of the problems associated with diagnostic error has been growing for more than 20 years, and ways to avoid these errors and patient harm have emerged from industry research and experience, hospitals have been slow to address the problem. Many say they simply don’t know where to start, and most have not yet taken action to improve diagnosis, resulting in a notable gap between the promise and rewards of knowledge-based improvement.
A new report from The Leapfrog Group, in partnership with the Society to Improve Diagnosis in Medicine (SIDM), aims to fill that gap by offering detailed guidance for 29 evidence-based actions hospitals can take now to improve diagnostic performance and prevent patient harm. Released in July, the report is an initial step in “Recognizing Excellence in Diagnosis,” a multi-year project funded by the Gordon and Betty Moore Foundation to advance diagnostic excellence in hospitals.
A survey of safety professionals from U.S. hospitals indicated gaps in execution and incentives for improving diagnosis. Results of the survey, which was distributed in 2016 to attendees of a Leapfrog webinar, revealed that although safety leaders knew that significant levels of misdiagnosis were likely occurring at their organizations, most had not yet taken action to address the problem.
At that time, inaction was attributed to insufficient commitment from executive leadership, a lack of performance measures for diagnostic error, and counterproductive financial incentives. Now, six years later, it is still true that the business case for diagnostic safety is lacking, and accreditation and government organizations are focused more on treatment and management issues than safety. Also, healthcare organizations have recently been distracted by COVID and changes in the practice environment, including telehealth and staffing issues related to burnout.
Results of the 2016 survey and recent experience indicates that awareness of the problem is not enough to overcome barriers and prompt organizations to address the problem.
Leapfrog Hospital Survey will include diagnosis in 2024
In addition to being valuable and relevant for all hospitals, the report and its 29 practices will serve as an early test of additions to the 2024 Leapfrog Hospital Survey. Hospitals volunteer to participate in the survey, which assesses hospital safety, quality, and efficiency based on national performance measures. The results are publicly reported, enabling hospitals to benchmark their performance as well as provide consumers with reliable assistance for choosing where to get care. The decision to include diagnosis in the annual survey—in which 2,300 hospitals currently participate—is expected to motivate hospitals and health systems to address diagnostic safety. Experts hope an element of competition regarding performance will move the needle on this long overdue safety initiative.
Missy Danforth, vice president of health care ratings at The Leapfrog Group, says publication of the report is an important step in the learning process. The 29 practices will be tested in a pilot survey of 100 or more hospitals this fall, with the findings to be reported in 2023. The results will help guide Leapfrog’s decision about which practices should be included in the 2024 hospital survey. Danforth also invites feedback from the community at large about the initial report.
She says, “We look forward to participating in a robust conversation among hospital leaders, risk managers, safety directors, patient and family advisory councils, and patient advocates.”
List of practices was developed by National Advisory Group
The practices highlighted in the report were selected by a national Advisory Group co-chaired by Hardeep Singh, M.D., M.P.H., a patient safety researcher at Center for Innovations in Quality, Effectiveness and Safety based at the Michael E. DeBakey VA Medical Center and Baylor College of Medicine, Houston; Mark L. Graber, M.D., SIDM founder and president emeritus; and Matt Austin, Ph.D., assistant professor, Armstrong Institute for Patient Safety and Quality at Johns Hopkins Medicine. In addition to experts in diagnosis, the Advisory Group includes Sue Sheridan, M.I.M., M.B.A. — founding director of Patients for Patient Safety US and SIDM’s first director of patient engagement — and payer representatives.
The group’s work began with an environmental scan that included a 2014–2021 literature review, interviews with experts in diagnosis, and results from hospital evaluation tools issued by The Leapfrog Group, The Joint Commission, and the Institute for Healthcare Improvement. This work resulted in a preliminary list of more than 300 potential practices or actions for improving diagnosis, from which the 29 featured practices were selected. All of the practices are evidence-based, and most have been recommended and endorsed in white papers and publications, including the 2015 report from the National Academy of Medicine, Improving Diagnosis in Health Care, and recent conclusions from AHRQ-sponsored research initiatives.
Practices reflect the need for improvement to systems and cognitive performance
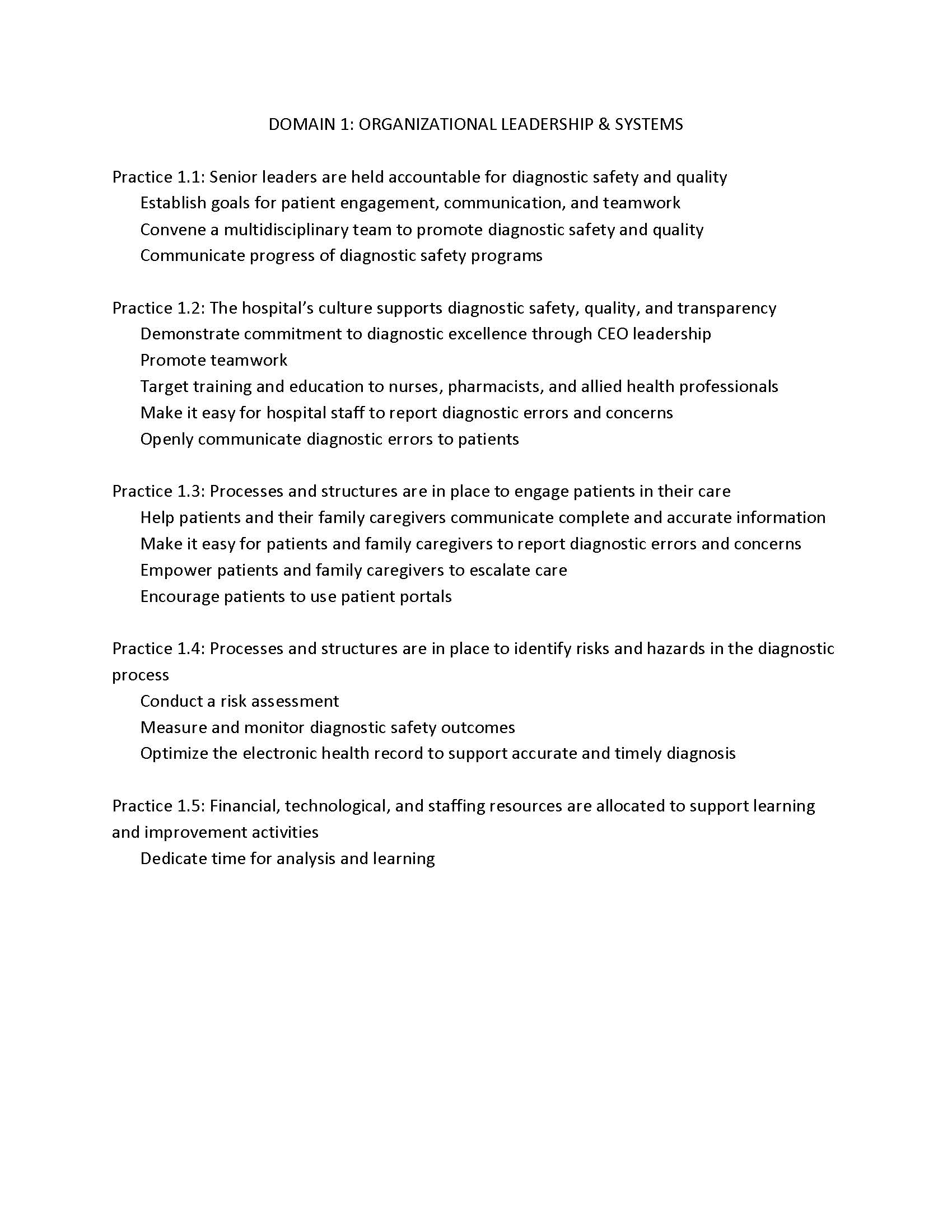
The new report presents the 29 recommended actions grouped under two domains: Organizational Leadership/Systems and the Diagnostic Process. (See sidebar). Just as leadership engagement is seen to be the key for safety improvement more generally, the report emphasizes that leaders’ involvement will be critical to improve diagnostic safety. Measures in this domain focus on leaders stating their intention to address diagnostic safety, promoting a culture of transparency and safety, and ensuring resources and staff time are available to work on specific projects. Hospitals are expected to find and learn from diagnostic errors and convene a multidisciplinary group to address issues identified. A host of new tools from the Agency for Healthcare Research and Quality have recently been published to assist in measuring diagnostic safety parameters.
The Leapfrog recommendations in the “Process” domain aim to improve diagnosis on the front lines. The many ways that cognitive errors can contribute to diagnostic errors are addressed by ensuring providers have adequate time for diagnosis and access to knowledge resources and decision-support tools that facilitate differential diagnosis. Other practices focus on improving communication, especially at handoffs, and facilitating access to consults and second opinions.
The practices also aim to improve patient engagement in the diagnostic process. For example, one of the practice recommendations is to “Make it easy for patients and family caregivers to report diagnostic errors and concerns”; other recommendations encourage the use of OpenNotes so that patients can see their own medical records and thus help ensure that test results, for example, don’t fall between the cracks. Another practice encourages hospitals to learn about diagnostic errors from their patients, citing a process developed by Kelly Gleason, Ph.D., R.N., and her team at Johns Hopkins for soliciting feedback about diagnosis from patients seen in the emergency department. Gleason’s work is highlighted in the report as a Featured Implementation Example.
Each of the 29 practice recommendations is presented along with a summary of its substantiating evidence, and examples of how the practice has already been adopted; organizations featured as exemplars include Geisinger, MedStar, Johns Hopkins, Baylor, Frederick Health, and Kaiser Permanente. To further support this effort, SIDM is developing new patient engagement tools and training materials to advance the adoption of these practices.
Helping turn knowledge into practice
Given the continued gap between understanding the problem of diagnostic error and tangible progress, frustration among long-time stakeholders and advocates is understandable. The National Academy report from 2015 identified diagnostic error as an urgent concern and outlined major recommendations to improve the diagnostic process and its outcomes.
“Now is the time to turn all of that knowledge into practice,” says Mark Graber. “We believe that organizations that implement the practices recommended in the Leapfrog survey will substantially reduce the harm that would otherwise result from the diagnostic errors involving their patients.”