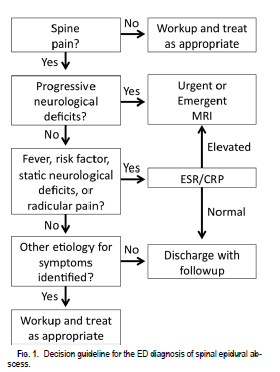
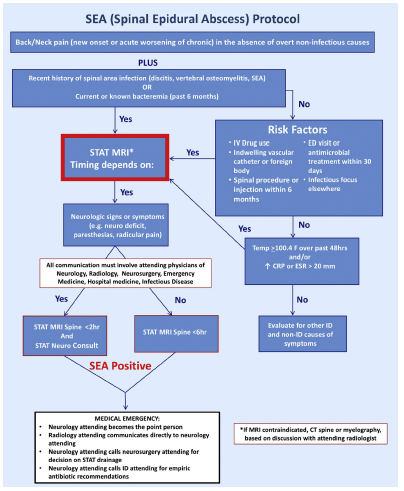
Overview of Diagnostic Algorithm
Standardize the approach to diagnosing spinal epidural abscess, a frequently missed diagnosis
Use of the diagnostic algorithm standardizes the approach to diagnosis of spinal epidural abscess. An organization can reduce the variability in the threshold for suspecting and deciding to pursue diagnostic imaging in patients with back pain. In addition, defining team member roles, communication and operational process steps can reduce delays in the diagnostic process.
The two images represented here are examples of diagnostic algorithms. These have been implemented in very few healthcare institutions.
Articles on diagnostic algorithms:
Feasibility/Logistics
Culture: A culture of eliminating variation and acceptance of group adherence to clinical guidelines would be a success factor in implementing this tool
Usability: User-friendly content that should be easily integrated into existing care delivery processes.
Infrastructure: No special infrastructure required. Can be disseminated and monitored using the existing leadership, communication, and tracking systems that exist in healthcare organizations.
Which stakeholders are essential for the tool to be implemented? Physician leaders of emergency medicine, hospital medicine and radiology are required stakeholders.
Implementation
Cost (human and technical): No additional cost, beyond what is usually incurred for rolling out clinical guidelines but there may be a large increase in imaging and its associated costs.
Location of usage (ambulatory vs inpatient): Highest yield would be Emergency Department, but could also be used by hospital medicine services and urgent care clinics
Roll out plan: Can be rolled out as a pilot in one emergency department and spread to multiple services or across a system
Post-Implementation Status
Current status (partly adopted or widely adopted): Not in widespread use.
Limitations: A standard approach eliminated variability, but evidence that use of the algorithm improves patient outcomes is lacking. Use of the algorithm is likely to increase the number of patients for whom MRI imaging is pursued. The correct number of imaging studies is not established and use of the algorithm could result in overuse.
Outcome measures: Unclear.
Sustainability/Viability: The first algorithm was published in 2011.
References
Davis DP et al, Prospective evaluation of a clinical decision guideline to diagnose spinal epidural abscess in patients who present to the emergency department with spine pain, Journal of Neurosurgery and Spine 2011;14:765-770
Madhuripan N et al, A Protocol-Based Approach to Spinal Epidural Abscess Imaging Improves Performance and Facilitates Early Diagnosis, Journal of the American College of Radiology 2018; 15(4): 648-51